“Every surgeon carries within himself a small cemetery, where from time to time he goes to pray—a place of bitterness and regret, where he must look for an explanation for his failures.” —Rene Leriche, The Philosophy of a Surgeon, 1951
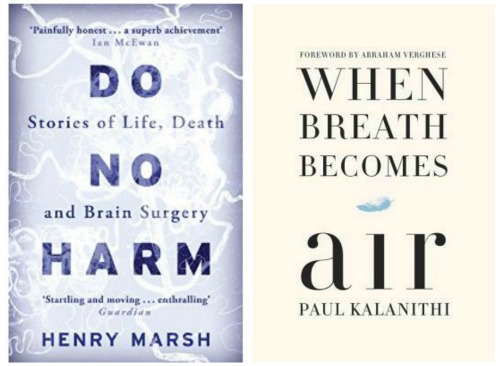
With this epigraph, Henry Marsh begins Do No Harm, a bittersweet memoir of his life as a neurosurgeon in the British National Health Service. This was one of two books I chose to read as we embark on a search for a new chair of neurosurgery at Montefiore and Einstein. As an endocrinologist, I have a limited familiarity with neurosurgery. Thinking that I should learn more about neurosurgery, and having been struck by recent reviews, I read both books, and found them much more than I had bargained for.
 In twenty-five chapters, each named for a memorable case he had operated on (pineacytoma, aneurysm, ependymoma, etc.), Marsh portrays vividly the unique challenges—medical, technical, ethical, philosophical—of this demanding surgical subspecialty. There’s lots of drama, but also fascinating technical details: e.g., his description of the operating microscope he employs, complete with its own armchair in which the neurosurgeon sits while performing the most-delicate procedures. Perhaps most affecting to me, though, is his description of the feeling of cognitive dissonance he experiences in operating on the most complex organ in the human body:
In twenty-five chapters, each named for a memorable case he had operated on (pineacytoma, aneurysm, ependymoma, etc.), Marsh portrays vividly the unique challenges—medical, technical, ethical, philosophical—of this demanding surgical subspecialty. There’s lots of drama, but also fascinating technical details: e.g., his description of the operating microscope he employs, complete with its own armchair in which the neurosurgeon sits while performing the most-delicate procedures. Perhaps most affecting to me, though, is his description of the feeling of cognitive dissonance he experiences in operating on the most complex organ in the human body:
“Are the thoughts that I am thinking as I look at this solid lump of fatty protein covered in blood vessels really made out of the same stuff? And the answer always comes back—they are—and the thought itself is too crazy, too incomprehensible, and I get on with the operation.”
Marsh’s path to becoming a neurosurgeon was anything but linear. After a series of seemingly random educational and work experiences, he takes a menial position as a “hospital porter.” The experience proves decisive. As he memorably writes: “Having spent six months watching surgeons operating, I decided this was what I should do. I found its controlled and altruistic violence deeply appealing.” Later in his medical training, observing a neurosurgeon clipping an aneurysm leads him to select this field for his life’s work.
His observations on the training of junior staff are trenchant. He captures a dilemma true of much of medical training but more acute in a field such as neurosurgery. Speaking of junior colleagues, he says: “If they do not take on difficult cases, how will they ever get any better?” But as he points out, the data clearly show that outcomes improve as a function of the neurosurgeon’s experience. Simulation training can take us only so far. Marsh feels an obligation to allow his junior colleagues to perform as much of a complex procedure as possible, but suffers greater anxiety watching them perform than when he himself is operating.
We train our medical students in how to convey “bad news,” but neurosurgery, as much as oncology, makes exorbitant demands in expecting practitioners to show appropriate sensitivity to patients and families when dealing with consequences such as paralysis, coma and death. Marsh illustrates this beautifully in juxtaposing a chapter on a patient with a large meningioma with one concerning his own infant son who turns out to have hydrocephalus caused by a rare, “benign” choroid plexus papilloma. “Anxious and angry relatives are a burden all doctors must bear, but having been one myself was an important part of my medical education.”
And this brings me to the second book, When Breath Becomes Air by Paul Kalanithi, a neurosurgery chief resident who wrote this memoir as he was dying from widely disseminated lung cancer. The slim volume is in two parts: the first, “In perfect health I begin,” is a recollection of his life for the thirty-six years before his diagnosis, and the second, “Cease not till death,” recounts the sombre details of his eighteen-month struggle. Kalanithi, the son of South Indian immigrants who, with the best intentions, ceaselessly pressured him and his brothers to succeed educationally and professionally, gratified their wishes. Stanford undergrad was a good start, but his love of literature led to a B.A. and then an M.A. in that subject, not exactly his physician father’s idea of the right path. But Kalanithi eventually concluded that he didn’t belong in an English department.
And so on to Yale Med School and a neurosurgery residency at Stanford. As with Marsh, his epiphany occurs observing a patient-doctor encounter, but for Kalanithi, with his love of words and meaning, it is not the technical wonder of watching a demanding neurosurgical procedure that convinces him. Instead, it is a conversation between a pediatric neurosurgeon and the parents of a child with a large brain tumor. Kalanithi chooses neurosurgery because he concludes that it presents “the most challenging and direct confrontation with meaning, identity, and death.” Knowing what awaits him six years later, do we still admire the courage of his conviction and strength of his ambition, or laugh with the Fates at his hubris? For me, that is the central question posed by this book, and the correct answer may be both of the above.
In retrospect, these two books had many lessons to teach me, but defining the qualities of an ideal chair of neurosurgery, perhaps unsurprisingly, was not among the primary ones. Perhaps I should just have consulted the AAMC’s William Mallon, who wrote “Seven Fresh Ideas to Help Searches for Academic Leaders.” His article begins on this discouraging note: “Why are academic recruitment searches such a source of complaint and consternation?” Certain generic, ideal qualities for a department chair—integrity, high moral and ethical values, a strong record of accomplishment in academic medicine and strong leadership skills—are obvious. But evidently, at least according to Mallon, finding individuals who embody all these traits is not easy, and that’s in part why so many academic medicine chair searches end badly.
What both books did teach me regarding a search for a neurosurgery chair is that finding a neurosurgeon with these ideal traits may be especially difficult. Could it be that the self-assurance required to cut into the “jelly” (by which Marsh signifies brain matter) is inconsistent with the need for a chair to look beyond personal ego gratification and foster the excellence of the academic health center as a whole? Marsh derisively describes neurologists, who along with neuroradiologists should be his most important colleagues, which suggests to me that he might not have been best suited to be a department chair. Kalanithi, exquisitely sensitive to patients and colleagues, a neurosurgeon/neuroscientist (how many of those exist?) and about to receive his first professorial appointment, might have become a superb chair. Sadly, we will never know.


Comments on this entry are closed.
Thank you very much for this moving and deeply insightful essay. I’m very grateful for this blog!