 EDITORS’ NOTE: The widespread use of antiretroviral therapy to suppress the HIV virus has helped tens of millions of people with HIV live healthier, longer lives. However, that increased life span has led to an increased risk of cancer. For 25 years, the AIDS Malignancy Consortium (AMC) has led national and international efforts to prevent and treat HIV-related cancers. Montefiore Health System and Albert Einstein College of Medicine have received a five-year, $111 million grant from the National Cancer Institute (NCI) to lead this research consortium.
EDITORS’ NOTE: The widespread use of antiretroviral therapy to suppress the HIV virus has helped tens of millions of people with HIV live healthier, longer lives. However, that increased life span has led to an increased risk of cancer. For 25 years, the AIDS Malignancy Consortium (AMC) has led national and international efforts to prevent and treat HIV-related cancers. Montefiore Health System and Albert Einstein College of Medicine have received a five-year, $111 million grant from the National Cancer Institute (NCI) to lead this research consortium.
Einstein’s director of multimedia communications, Sunita Reed, discussed the grant and its significance for people living with HIV—and all cancer patients—with Joseph Sparano, M.D., associate chair for clinical research in the department of oncology at Montefiore, associate director for clinical research at the NCI-designated Albert Einstein Cancer Center, and principal investigator on the grant.
This transcript has been edited for clarity.
What major gains have there been in managing HIV in the U.S., and what challenges remain?
There are about 38 million people worldwide living with HIV infection, including over one million in the United States. The survival rate for people living with HIV has improved dramatically over the last 20 years. With improved antiretroviral therapy, it’s turned HIV infection from an acute illness to really one that is more of a chronic condition. People living with HIV are living long, relatively healthy lives. As the population of patients living with HIV increases, they can develop conditions that typically occur with age. One of those conditions is cancer. In fact, cancer is emerging as a major cause of death in people living with HIV—not necessarily complications from their HIV infection.
Why do people with HIV have an increased risk of certain cancers?
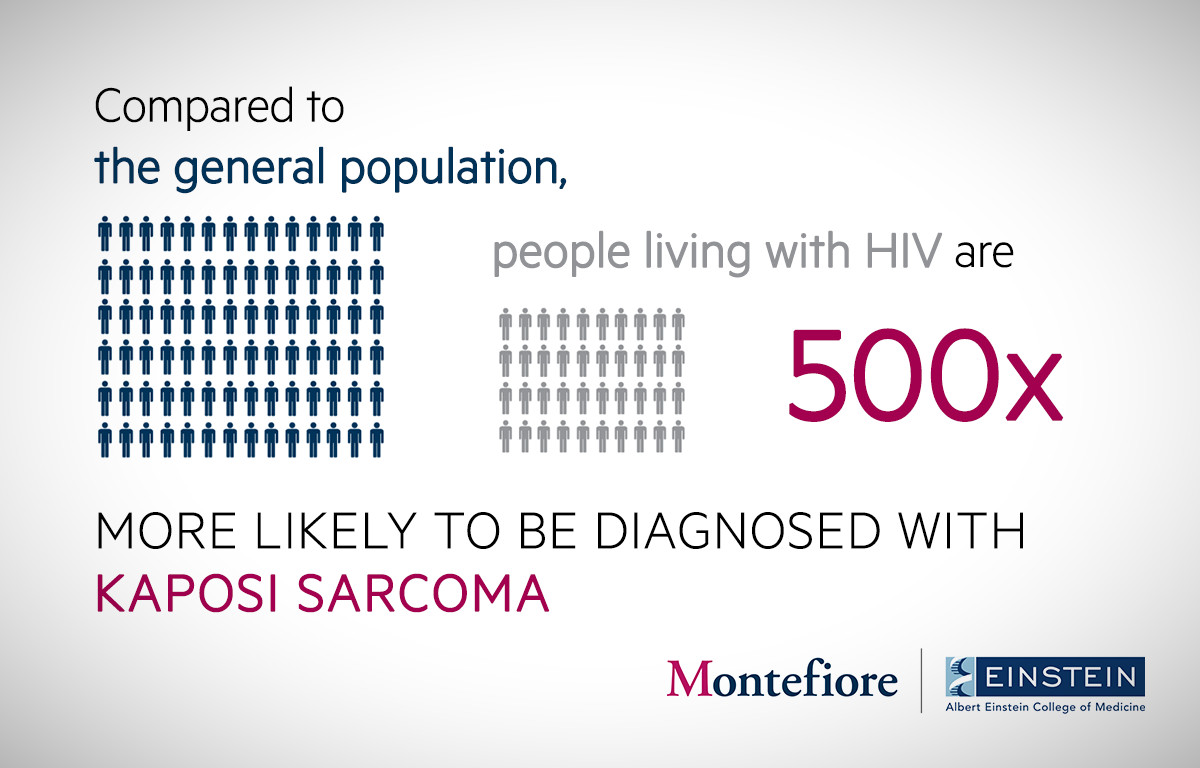
People living with HIV infection are at an increased risk of cancer for several reasons. First, as they live longer, they’re more susceptible to diseases that are typically associated with aging, such as cancer. Second, people living with HIV have higher smoking rates, which are associated with higher rates of lung cancer, head/neck cancer, and a variety of other cancer types. Third, people living with HIV are more likely to have been exposed to viruses that can induce cancer, especially the human papillomavirus, or HPV virus, which is very prevalent in the general population and also prevalent in patients with HIV infection. However, people with HIV are more likely to develop HPV-associated cancers as a consequence of their underlying HIV infection because of the immune suppression that may occur in the context of HIV infection.
Can you tell us about your new role leading the AIDS Malignancy Consortium, and why Montefiore and Einstein are well positioned to lead this effort?
It was recognized many years ago that people living with HIV had higher cancer rates, and that the treatment and prevention of cancer in people living with HIV pose particular challenges. So the National Cancer Institute established a network of organizations funded specifically to study the prevention and treatment of cancer in people living with HIV. That group is called the AIDS Malignancy Consortium. The mission of the AMC is to reduce the burden of cancer in people living with HIV in terms of the likelihood of getting cancer and the death rates associated with cancer in those patients. It started out as a national organization based in the U.S. with a consortium of about 25 centers, and now has expanded into a global organization, including centers in Africa and Latin America and about 45 sites worldwide.
For the past 14 years, I’ve served as the AMC vice chair, and I’m now moving into the position of the group chair. The researchers at Einstein and the clinical care provided by Montefiore mean that both organizations are uniquely suited to play a leadership role in this organization because of their expertise in the treatment of HIV infection. Einstein is one of a handful of centers funded by the National Institutes of Health noted specifically for its research efforts in HIV. It’s also funded by the National Cancer Institute specifically to do cancer research.
The Bronx is home to 1.5 million people. It’s a multiracial, multiethnic community where 27% of the residents live at or below the poverty line. It has some of the highest rates of HIV infection in the country. Because of that, there’s a high cancer burden, both in the context of HIV infection and even in individuals who don’t have HIV. We’re particularly focused on trying to serve the needs of the community by not only providing high-quality care for both cancer and HIV infections, but doing it in a multidisciplinary, coordinated, compassionate way. We also offer the latest research and therapeutic advances in terms of preventing disease, and look forward to expanding the reach of what we’re already accomplishing in this community.
Will you study the health of children or only adults?
HIV infection is uncommon in children in the U.S., but it’s a major problem in other areas of the world, particularly Africa. Kaposi’s sarcoma, a potentially deadly form of skin cancer, is very common in children in Africa. This disease is actually caused by a virus, a human herpes virus. Our group is now trying to develop therapeutic strategies that are effective and nontoxic, that can address this critical problem in Africa.
Can you give us an example of the AMC’s research in adults living with HIV?
One example would be the ANCHOR trial. This is a large trial of 5,000 patients who have HIV infection and who also have high-grade anal dysplasia—a precancerous lesion in the lining of the anal canal that can be detected only by a procedure that requires individuals who are specially trained to perform it. It is the first trial ever of its kind to screen people at high risk for anal dysplasia, identify it, and treat it to see if we can prevent anal cancer from ever occurring in the first place. This is an example of the AMC doing things that are very difficult for other groups to accomplish. It’s important to understand that some of the discoveries and advances that have been made by the AMC over the last 25 years have impacted the prevention and treatment of cancer not only in people with HIV, but also in individuals who don’t have HIV infection. Our group has particular expertise in testing therapeutic vaccine strategies to treat HPV-associated cancers. I think some of this work will ultimately have an impact on the management and prevention of cancers in individuals who don’t have HIV infection.

