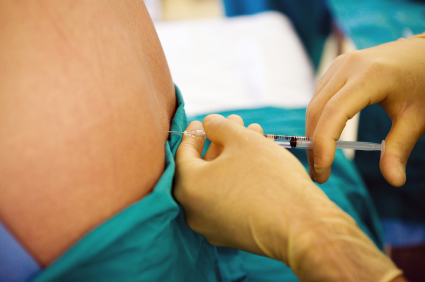
 Recent coverage of a deadly fungal meningitis outbreak tied to an injectable epidural steroid used for back pain has made front-page news. The New York Times and other media outlets have run articles tracing the contaminated substance known as methylprednisolone acetate to a Massachusetts compounding manufacturer. While the media have focused mostly on the lamentable lack of FDA oversight of this company and the “compounding” field it represents, I was struck by this comment:
Recent coverage of a deadly fungal meningitis outbreak tied to an injectable epidural steroid used for back pain has made front-page news. The New York Times and other media outlets have run articles tracing the contaminated substance known as methylprednisolone acetate to a Massachusetts compounding manufacturer. While the media have focused mostly on the lamentable lack of FDA oversight of this company and the “compounding” field it represents, I was struck by this comment:
Patients most likely assumed there was strong evidence that the procedure itself works. But the Cochrane Collaboration, an international group of medical experts, reviewed the data last year and found there was “no strong evidence for or against” the injections. Patients exposed to the drug in the current outbreak may have risked their health or even their lives for an elusive goal.
This underscores a concern I’ve long had about most discussions of healthcare delivery and financing: the lack of focus on Americans’ insatiable desire for expensive, invasive, and often unproven treatments. The truth is, a lot of the stuff we provide in medical care is based on conjecture, experience, and anecdote rather than real evidence.
Now, as a proponent of what’s known as “evidence-based medicine,” I hasten to admit that high-quality evidence isn’t available to assess the efficacy of many of the things doctors do to respond to patients’ symptoms, illnesses, and concerns. Doctors should respond to their patients’ needs, and this will sometimes (perhaps often) involve actions that have not been proven to be effective. Indeed, that’s why medicine is so often described as a science and an art, and why hewing only to reductionist or epidemiologic scientific methodologies doesn’t get you where you need to go.
We need physicians who are not guided only by science, but who understand and incorporate science as part of clinical decision making.
When treatments carry the risk of harm (as virtually all allopathic treatments do), policy makers will often look at the “risk-benefit ratio” as a way to assess whether the harms that may be caused by the intervention could outweigh the benefits anticipated. When looking at this ratio, it is critical to recognize that it is influenced not only by the numerator (the risks or harms) but also by the denominator (the benefits). It is obvious that as risk goes up, so does the risk-benefit ratio; but for any given degree of risk, it also goes up as benefit goes down. What this means is that if a treatment is not very likely to be beneficial, even a very small amount of risk may be unacceptable. Taken to its extreme: a treatment with no benefit at all will have a ‘zero tolerance’ for risk: there is essentially no amount of risk that is acceptable when providing a useless treatment.
While I applaud the Times’ highlighting this important lack of regulatory oversight involving the injectable steroid, I think the tragedy is compounded by this unproven treatment having apparently been so widely used. From the article: “In 2011, 2.5 million Medicare recipients had the injections, as did an equal number of younger people, according to Dr. Ray Baker, president of the International Spine Intervention Society.”
As of the writing of this post, more than 13,000 people in 10 states have reportedly been exposed to the drug lot that was apparently contaminated with fungus, with 137 individuals known to be infected and 12 who have died as a result. These numbers are almost certain to be higher by the time you read this.
Now, from a purely statistical perspective, the probability of infection is low: if reliable estimates put the number of yearly injections (Medicare and non-Medicare) at 5 million and 137 people get infected, that’s only a 0.003% chance of getting sick from the shot. Sometimes you’ve got to accept that treatments have some risks as you seek to reduce suffering or improve outcomes; if we had a treatment that could cure your cancer but caused serious (even life-threatening) infections 3 times out of 100,000, you’d opt for that treatment in a New York minute. But if the treatment doesn’t actually work, no amount of risk is tolerable.
It would be nice if our conversations about healthcare financing could include a rational discussion, rooted in evidence-based medicine, of reining in the costs of healthcare delivery. That would put limits on the sorts of dubious procedures that continue to be covered by insurance companies despite a lack of demonstrated benefit—and could reduce patients’ exposure to useless, expensive, and potentially harmful medical treatments.


Comments on this entry are closed.
Hello,
First of all I want to say thanks for this nice article,
In my humble opinion I totally agree with the concept of “risk benefit ratio” but, sometimes the doctor can take the decision to give his patient a certain medications even with It’s high risk ratio if he believe it could make a good change and with the patient’s acceptance off course!
As a recent recipient of the above mentioned injections (for the 5th time), I have had 50% relief; however,
this last set of injections has had no effect. At 81 years of age, I will not agree to further injections after
reading the above article. I do wish to thank you for the honest assessment of the proceedure. J. Conley
I am new to your blog. I have had a few patients with these kinds of injections, and though I practice in Canada, the issues are universal. I look forward to reading future posts.
Fortunately, my experience with evidence-based medicine in working with my doctor to treat my Complex Regional Pain Syndrome has been positive. This is such an unfortunate incident and definitely a cautionary tale.