 Even the healthiest among us who are lucky enough to live long lives will break down and, ultimately, shut down. We age; we die. Yet this seemingly unavoidable process will likely change in the foreseeable future.
Even the healthiest among us who are lucky enough to live long lives will break down and, ultimately, shut down. We age; we die. Yet this seemingly unavoidable process will likely change in the foreseeable future.
In recent years, the prospect of curbing aging has gained traction, increasing not only the average human life span but the maximal human life span, which has thus far steadfastly remained at roughly 115 years. Surprisingly, much of the interest and excitement stem from nontraditional aging research.
Age-related deterioration is due largely to the complex and numerous forms of damage that occur over time to the macromolecules, such as DNA, proteins and lipids, that make up our bodies. Despite the complexity of age-related damage, the aging process has become increasingly better defined during the last two or three decades. This has led many researchers to explore the use of pharmacological approaches to potentially slow the accumulation of macromolecular damage, with the hope that drugs could one day have broad beneficial antiaging effects.
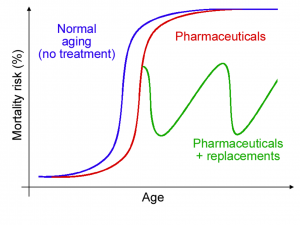
Traditional research aimed at combating the effects of age has focused on using pharmaceuticals, which may improve the average—but not likely the maximal—life span. Replacement strategies, especially when applied cyclically, have the potential (either alone or in combination with pharmaceuticals) to reverse aging and extend the maximal life span. (Image courtesy of Jan Vijg.)
This ambitious plan might eventually be used to slow certain aspects of aging. However, due to the enormous complexity of the macromolecular damage that occurs, new drugs are likely to increase only the average life span (by reducing the risk of age-related diseases) without significantly increasing the maximal life span. And pharmaceuticals are not likely to reverse age-related damage once it occurs.
Don’t Repair—Replace
Replacement of cells, tissues and organs—a relatively new and expanding research area—provides a potentially more straightforward and immediate, albeit nontraditional, approach to reversing age-induced damage.
To use an old car as an analogy: it is much easier to keep it running in top form by simply replacing parts as needed than by trying to undo the rust and corrosion on its parts. We are, of course, more complicated than cars. Nevertheless, the replacement of parts in humans has already been going on for quite some time. Today just about every organ and tissue in the body has been successfully transplanted from one individual to another. But these body parts and organs, of which there is a chronic shortage, have come from donors, often deceased, and are generally used to treat patients in dire need. So organs and tissues that come from donors are not a valid source for the treatment of aging individuals who are otherwise disease-free.
Growing Solutions to Aging
This is where recent advances in lab-grown organs come into play. Among other researchers, Anthony Atala and his group at Wake Forest have been growing organs for transplantation with remarkable success. For example, as early as 1999 they grew bladders in their labs using cells from the very same patients who then received the lab-grown bladders. These performed remarkably well. Other organs and body parts are also being grown in research labs throughout the country with the goal of using them for transplantation in patients. The cells in these organs, and therefore the organs themselves, can be free of age-related damage when they are grown from young or embryonic cells.
Impressive strides are also being made in developing non-cell-based artificial organs and limbs, which may soon outperform those we were born with. As with an old car, replacing parts in people appears to be simpler than repairing the long list of types of macromolecular damage. With replacements, all forms of damage in a tissue are gone in one fell swoop.
A “New” Brain
But all these replacements are of little use if we end up with an old, senile brain in a rejuvenated body. The brain as a whole organ is not replaceable, for obvious reasons. On the other hand, at the cellular level, replacements for the brain without loss of self-identity appear possible if done progressively, over time. The neocortex, the part of our brains that we use to think and that largely defines who we are as individuals, is remarkably plastic. In classic sensory-deprivation experiments done across species from mice to primates, areas of the neocortex were found to be reallocated to new functions over time based on need. Even under normal circumstances, changes in our neocortical maps occur continuously on a smaller scale as we go through life acquiring new knowledge and skills. One of the more dramatic examples of neocortical plasticity can be found in aging humans who have slow-growing benign gliomas, which typically take four to eight years before being diagnosed and which destroy the speech areas of the neocortex. In these individuals, the language functions relocate to new neocortical areas without any noticeable disruption in speech. So if the cellular substrate for functions as complex and dear to us as language can change over time, neocortex regeneration, if done slowly, is—in theory—possible.
Cell replacement for the neocortex also seems possible in practice. Recent studies show that young neocortical cells transplanted into the neocortices of adult mice are, at least to the extents examined so far, functionally incorporated into the existing circuitry. Although these studies support the feasibility of progressively replacing cells in the neocortex, major questions remain unaddressed. For example, there are many cell types, neural and non-neural, that are required for normal neocortical function. Cells of all types will need to be replaced and their organization maintained to completely undo the damage caused by aging. Therefore, we will need to test for optimal combinations and arrangements of cells. Other questions related to the size of the human neocortex, the complexity of connections between transplanted cells and brain areas and the rates at which new cells should be transplanted also remain to be addressed. Nevertheless, techniques already exist today that allow us to address these questions. Optimism about cell replacement as a means of brain rejuvenation would seem justified.
There is increasing interest and investment in anti-aging research in both academia and industry. Although these sectors do not yet consider replacements part of their arsenal for combating aging and its related diseases, the advent of new cell, tissue and organ transplants will make the transition in this field’s focus inevitable.

